As pediatric surgeons, we specialize in the care of infants, children, and adolescents, who require surgery for common conditions identified by their primary care providers. These conditions can often be treated with minimally invasive surgery.
Our qualified pediatric surgeons perform minimally invasive procedures through small incisions instead of one large incision, which can lead to quicker recovery times and less pain than conventional surgery.
Learn more about the conditions we treat below or contact us online for more information.
- Hernias
- Head and Neck Surgery
- Oncology
- Chest Wall Deformities
- Inflammatory Bowel Disease
- Gastrointestinal Surgery
- Complex Thoracic Surgery
- Neonatal Surgery for Fetal Diagnoses
- Liver and Gallbladder Surgery
- Anorectal Malformations
- Pediatric Trauma
- Skin Masses and Infections
- Genitourinary
- Gynecology
- Breast Disorders
Hernias
What is an umbilical hernia?
An umbilical hernia is a bulge or protrusion that is seen or felt in the area of the belly button. This bulge is the result of a failure of the abdominal wall to completely close during development, leaving an opening for a portion of the intestine and fluid to come through. Umbilical hernias are present at birth but may become more noticeable during times when your child is bearing down – crying, coughing, or straining to have a bowel movement. The bulge may seem to disappear when the child is quiet or resting. Umbilical hernias do not usually cause pain.
Most umbilical hernias (about 90 percent) close on their own by the time the child is 4-5 years old. Therefore, your surgeon may recommend waiting until your child is 4-5 years old before undergoing a surgical repair. Waiting has benefits even if the hernia does not close on its own. The hernia generally gets smaller, which simplifies the repair procedure. Waiting also allows the muscle wall to thicken and mature, which makes the repair more robust.
In some cases, such as a large hernia or incarceration, infant hernia repair surgery may be recommended prior to 4-5 years of age. Incarceration of the hernia occurs when the intestine gets trapped in the defect and is unable to go back into the abdomen.
An incarcerated hernia will often cause a painful, firm, discolored bulge. If your child has signs of an incarcerated hernia, he or she should be brought to the Emergency Department for immediate evaluation by a medical professional to prevent any damage to the intestines.
It is estimated that umbilical hernias occur in 10-15 percent of all infants, with boys and girls affected equally. African Americans, low birth weight and premature infants are at a greater risk for having an umbilical hernia. How the umbilical cord is clamped or cut after birth has no effect on whether an umbilical hernia will develop or not develop.
Evaluation and diagnosis
The diagnosis of an umbilical hernia is confirmed by a thorough health history and physical examination. Imaging studies are almost never needed to diagnose umbilical hernias.
Treatment for umbilical hernia
If your child’s umbilical hernia does not close on its own by the time he or she is 4-5 years old, we will recommend umbilical hernia surgery for your child. Visit our Guide to Your Child’s Surgery to learn more about what to expect when your child has surgery at The Children’s Hospital of Philadelphia.
Surgical repair of umbilical hernia
Umbilical hernia surgery is a day surgery, meaning your child will go home the same day as the procedure. The procedure will be done under general anesthesia.
A small curved incision (resembling a smile) will be made under your child’s belly button. The opening will be closed, usually with absorbable sutures, and the overlying skin will be closed with a combination of absorbable stitches below the skin and DERMABOND. If DERMABOND is not used, your child may have a dressing over the site, which should be removed 48 hours after surgery.
DERMABOND is a sterile, liquid adhesive that will hold the edges of your child’s wound together and act as a waterproof dressing. It usually stays in place for 5-10 days before it starts to fall off. You should not pick, peel or rub the DERMABOND, as this could cause your child’s wound to open before it is healed.
Once it sets, the adhesive can get wet (as in a shower) the same day as the procedure, but should not routinely be submerged under water (as in swimming) for 5-10 days. Do not apply any ointments such as Vaseline or Neosporin to the incision while the DERMABOND is in place.
Follow-up care
Hernia surgery recovery is relatively straightforward. After surgery, your child’s belly button may appear to be slightly swollen, but this will go away over the next few weeks. Your child will not be able to participate in physical education or sports for 2-3 weeks after surgery. We will schedule your child for a follow-up appointment 2-4 weeks after the procedure, at which time we will evaluate the repair and your child’s recovery.
Even after repair, there is a very small risk of recurrence of the hernia. If it appears that your child’s hernia has come back at any point, please make an appointment with your doctor to be evaluated.
When to call the doctor
Seek medical care immediately if your child has any signs or symptoms of incarceration:
A hernia that is stuck out and not able to be reduced (gently pushed back into the abdomen)
A painful, firm, discolored bulge
Please call the Division of Pediatric General, Thoracic and Fetal Surgery at 215-590-2730 if your child has any of the following symptoms:
Fever (a temperature of 101.5 degrees or higher)
Any signs of infection, including redness, swelling or pain
Any drainage from the incision
Any pain that is not controlled with the prescribed pain medicine
A bulge at the belly button
Any further questions or concerns
What is an inguinal hernia?
An inguinal hernia is usually identified as a bulge or swelling in the groin. In boys this protrusion often extends into the scrotum. The hernia itself is not the bulge, but rather a hole that allows contents from the abdomen to pass into the groin.
When the hole is small and only allows fluid to pass through, it is called a hydrocele. When the hole is larger, the intestines or other organs are able to pass into the groin. While inguinal hernias are present at birth, they may not become noticed for days to years, and they are most easily identified when your child is straining, crying or coughing.
The bulge may seem to resolve when the child is relaxed or resting, and there is rarely any discomfort from the hernia.
If an inguinal hernia is present, there is no chance the body will close the hole. Umbilical hernia surgery is required to prevent complications from occurring. Your surgeon may recommend waiting until your child is at least 6-8 weeks old before undergoing surgical repair, as this is a very safe outpatient procedure for kids at that age.
As many as 20-30% of children with an inguinal hernia may have an unidentified hernia on the opposite side, so your child’s surgeon may recommend inserting a small camera into the hole during the operation to check if another hernia is present. If so, it can be repaired while your child is already under anesthesia.
In rare cases, the intestines may become stuck and unable to pass backwards through the hole and into the abdomen. When this occurs, the bulge you see may become very firm and red. This is called incarceration of the hernia, and your child may develop pain, vomiting and/or become inconsolable.
Many of these situations require emergent operations so if these signs and symptoms are present, your child should be brought to our office or the Emergency Department for immediate evaluation.
Evaluation and diagnosis
The diagnosis of an inguinal hernia is usually suggested by the history of a groin bulge that comes and goes. The hernia can be confirmed by a physical examination, and our surgeons rarely require additional testing. If any question exists about the presence of an inguinal hernia, an ultrasound can be performed to assist with the diagnosis.
Treatment for Inguinal Hernia
Once the diagnosis of an inguinal hernia is confirmed, we will recommend a hernia repair surgery. There are no medications or alternative therapies available. It is fine to encourage full activities for your child until the time of the operation, and there is no need to limit them in any way.
Surgical repair of inguinal hernia
Inguinal hernia is one of the most common conditions we treat. The surgery to repair an inguinal hernia is an outpatient procedure, meaning your child will go home a few hours after the operation. The procedure will be done under general anesthesia.
A small incision is made in the groin, and the hole is closed with sutures. Prior to closing the hole, your surgeon may insert a camera to see if a hernia is present on the opposite side. We don’t use mesh or screens like you may be familiar with in adult hernia operations, and children recover from this procedure much faster than adults. The sutures we use eventually dissolve, so your child will not need to have any stitches removed.
When the operation is over we cover the wound with small stickers called Steri-Strips, followed by gauze and a clear waterproof dressing. Alternatively, we may apply a skin glue called DERMABOND which is a liquid adhesive that will hold the edges of your child’s wound together and act as a waterproof dressing. It usually stays in place for 5-10 days before it starts to fall off. Your child should not pick, peel or rub the DERMABOND, as this could cause their wound to open before it is healed.
Your child may shower or receive a sponge bath the day after surgery, but they should avoid submersion (bath or swimming) for a week to 14 days. Do not apply any ointments such as Vaseline or Neosporin to the incision while the DERMABOND or dressing is in place.
Follow-up care
When you are home after your child’s surgery, give them ibuprofen or acetaminophen for any discomfort during their hernia surgery recovery. We allow them to resume normal activities such as running and playing, although most children are a bit sleepy on the day of the procedure. Your child’s groin may become slightly swollen or bruised, and this will go away over the next few weeks. We will schedule your child for a follow-up appointment 2 weeks after the procedure to ensure everything is going well.
Even after repair, there is a very small risk of recurrence of the hernia. If it appears that your child’s hernia has come back at any point, please make an appointment with your doctor to be evaluated.
When to call the doctor
If your child is awaiting surgery for an inguinal hernia, seek medical care immediately if your child has any signs or symptoms of an incarcerated hernia. If the operation has already occurred, please call our office for any of the following:
Fever (a temperature of 101.5 degrees or higher)
Any signs of infection, including redness, swelling or increased pain
Drainage from the wound
Pain that is not controlled with the recommended pain medicines
WHAT IS AN EPIGASTRIC HERNIA?
Small openings in the abdominal connective tissue between the breast bone and the umbilicus (belly button) can occur naturally. The opening allows internal fat or bowel to push out into the tissue under the skin when the child strains. This is an epigastric hernia.
EVALUATION AND DIAGNOSIS
An epigastric hernia is best seen with the child’s arms raised and the back in a slight back-bend. Parents often first identify the hernia while helping the child to change their shirt or giving them a bath.
TREATMENT FOR EPIGASTRIC HERNIA
Unlike umbilical hernias that may resolve up to 4 years of age, epigastric hernias do not go away on their own. Elective outpatient pediatric hernia surgery may be recommended. Occasionally, the hernia can cause pain.
SURGICAL REPAIR OF EPIGASTRIC HERNIA
The surgery to repair an epigastric hernia is an outpatient procedure, meaning your child will go home a few hours after the operation. The procedure will be done under general anesthesia.
A small incision is made overlying the hernia, and the hole is closed with sutures. We don’t use mesh or screens like you may be familiar with in adult hernia operations, and children recover from this procedure much faster than adults. The sutures we use eventually dissolve, so your child will not need to have any stitches removed.
When the operation is over we cover the wound with small stickers called Steri-Strips, followed by gauze and a clear waterproof dressing. Alternatively, we may apply a skin glue called DERMABOND which is a liquid adhesive that will hold the edges of your child’s wound together and act as a waterproof dressing. It usually stays in place for 5-10 days before it starts to fall off. Your child should not pick, peel or rub the DERMABOND, as this could cause their wound to open before it is healed.
Your child may shower or receive a sponge bath the day after surgery, but they should avoid submersion (bath or swimming) for a week to 14 days. Do not apply any ointments such as Vaseline or Neosporin to the incision while the DERMABOND or dressing is in place.
FOLLOW-UP CARE
When you are home after the surgery, give your child ibuprofen or acetaminophen for any discomfort. We allow them to resume normal activities such as running and playing, although most children are a bit sleepy on the day of the procedure. They area may become slightly swollen or bruised, and this will go away over the next few weeks. We will schedule your child for a follow-up appointment 2 to 4 weeks after the procedure to ensure everything is going well.
Even after repair, there is a very small risk of recurrence of the hernia. If it appears that your child’s hernia has come back at any point, please make an appointment with your doctor to be evaluated.
WHEN TO CALL THE DOCTOR
After repair of an epigastric hernia, please call our office for any of the following:
Fever (a temperature of 101.5 degrees or higher)
Any signs of infection, including redness, swelling or increased pain
Drainage from the wound
Pain that is not controlled with the recommended pain medicines
Our surgeons have the expertise to fix any and all types of abdominal wall hernias, including inguinal hernias, umbilical hernias, epigastric hernias, and less common hernias such as parastomal or ventral hernias. If you have any questions about your child’s surgery, please call us at (512) 456-9423.
Head and Neck Surgery
Our team of pediatric surgeons specializes in the surgical management of various head and neck lesions. Whether the symptoms are congenital or acquired, our pediatric surgeons take great care to fully treat your child’s unique needs.
Learn more about some of the most common procedures we perform or contact us if you have any specific questions about your child’s appointment.
What is it?
A thyroglossal duct cyst (TDC) is the most common congenital neck lesion observed in children. The thyroglossal duct is a remnant of the developing thyroid gland. When the thyroid gland is developing it begins as a group of cells at the base of the tongue. During development these cells move down the neck through a canal called the thyroglossal duct. This duct normally involutes or disappears once the thyroid gland reaches its final position in the neck. If the duct does not fully disappear, portions of the duct remain leaving cavities or pockets called cysts.
Signs and Symptoms
Thyroglossal duct cysts normally present as a painless swelling near the midline of the upper neck. These cysts may move with swallowing or with tongue protrusion. These cysts can become infected causing redness and tenderness.
Diagnosing
Generally, diagnosis is made by physical exam. An ultrasound may be performed to evaluate the cyst and to confirm the presence of a normal thyroid gland.
Treatment
Surgery to remove the cyst is the definitive treatment. If an infection is present, the infection will need to be treated before the surgery can be performed. The surgery is performed under general anesthesia. The operation is called the Sistrunk procedure. An incision is made over the cyst. The cyst, the entire thyroglossal duct tract and the central portion of the hyoid bone (a small horseshoe-shaped bone that is found in the neck below the chin) are removed. The surgery normally lasts 1-2 hours. Your child may be able to go home after the procedure or may stay overnight. A drain may be left in place. The risk for recurrence is approximately 10%.
Follow up care
Instructions for wound care and postoperative activity will be given to you by your surgeon. Postoperative pain can normally be managed with acetaminophen (Tylenol) and/or ibuprofen (Motrin). Your child will be scheduled for a follow up appointment 2-4 weeks after the procedure.
What is it?
The branchial arches represent the embryological precursors of the face, neck and throat. Adjacent to each arch is a cleft. Anomalies of the branchial arches and clefts are the second most common congenital lesions of the head and neck in children. They may present as cysts, fistulas or cartilaginous remnants.
Signs and Symptoms
The most common presentation for a branchial cleft is a small skin opening (fistula) or painless swelling (cyst) in the lower anterior or lateral region of the neck. If a fistula is present there may be small amounts of clear fluid that intermittently drain.
Diagnosing
Generally, diagnosis is made by physical exam. An ultrasound, CT scan or MRI may be needed if the diagnosis is unclear.
Treatment
Surgery to remove the cyst or sinus is the definitive treatment. If an infection is present, the infection will need to be treated before the surgery can be performed. The surgery is performed under general anesthesia. An incision is made either over the cyst or around the fistula. Occasionally more than one incision is needed to remove a fistula. The surgery normally lasts 1-2 hours. Your child may be able to go home after the procedure or may stay overnight. A drain may be left in place. The risk for recurrence is less than 10%.
Follow up care
Instructions for wound care and postoperative activity will be given to you by your surgeon. Postoperative pain can normally be managed with acetaminophen (Tylenol) and/or ibuprofen (Motrin). Your child will be scheduled for a follow up appointment 2-4 weeks after the procedure.
What is it?
The thyroid gland is a butterfly shaped organ found in the neck. The thyroid gland produces thyroid hormone which regulates the body’s metabolic rate as well as heart and digestive function, muscle control, brain development mood and bone maintenance. Problems with the thyroid gland include thyroid nodules (abnormal growths), hyperthyroidism (overactive gland), and hypothyroidism (underactive gland).
Signs and Symptoms
Thyroid nodules commonly present as painless “lumps” either seen or felt in the neck. Symptoms of hyperthyroidism include irritability, insomnia, nervousness and tremors. Symptoms of hypothyroidism include fatigue, weakness, weight gain and depression. Both hyperthyroidism and hypothyroidism can cause enlargement of the thyroid gland (goiter).
Diagnosing
Thyroid nodules are commonly diagnosed with a physical examination and an ultrasound. The concern with thyroid nodules in children are that they may harbor a thyroid cancer. A needle biopsy may be recommended. Hyperthyroidism and hypothyroidism are usually diagnosed by blood tests. Most children with thyroid problems are first referred to a pediatric endocrinologist.
Treatment
Surgery may be recommended for certain thyroid diseases. The surgery may involve a total thyroidectomy (removing the entire thyroid gland) or a lobectomy (removing one half of the thyroid gland). Risk for thyroid surgery include injury to the parathyroid glands and the laryngeal nerves. Surgery normally lasts 1-2 hours. Your child will normally stay in the hospital at least overnight. A drain may be left in place. If the entire thyroid gland is removed your child will be placed on thyroid hormone replacement, supplemental calcium and vitamin D after the surgery.
Follow up care
Instructions for wound care and postoperative activity will be given to you by your surgeon. Postoperative pain can normally be managed with acetaminophen (Tylenol) and/or ibuprofen (Motrin). Your child will be scheduled for a follow up appointment 1-2 weeks after the procedure.
Tongue-tie, or ankyloglossia, is a condition in which a child is born with too short of a tissue connecting the tongue to the bottom of the mouth. In this instance, a simple pediatric tongue-tie surgery can be performed to release the tongue from the constricting tissue.
Child tongue-tie surgery is a relatively simple procedure that can be done under general or local anesthesia, depending on the infant’s age, followed by acetaminophen (Tylenol) for pain or discomfort during the healing process.
Oncology
Pediatric surgical oncology can provide essential treatment for your child. Regardless of the type of cancer or tumor, our team of pediatric oncology surgeons will provide the utmost care and skill for your child’s procedure.
As pediatric oncological surgeons, we treat a wide variety of tumors that can be found throughout the neck, chest, and abdomen. These include but are not limited to:
- Wilms’ Tumor
- Neuroblastoma and other adrenal tumors
- Pancreatic tumors
- Hepatoblastoma and other liver tumors
- Soft tissue sarcomas
- Thyroid tumors
- Thoracic Tumors
At Austin Pediatric Surgery, our goal is to be the best providers for pediatric surgery and care, which includes in-depth information about what to expect from your child’s condition and procedure. Read more about some of the most common oncological surgeries we perform or contact us for additional information on your child’s procedure.
What is it?
Neuroblastoma is a type of solid organ cancer in children that comes from the adrenal glands (an organ that sits on top of kidney and secretes hormones and other important chemicals) and the sympathetic nervous system (nerve cells). Neuroblastoma is:
- the most common abdominal tumor in children
- has an incidence of greater than 600 cases in the United States a year
- can occur in the head and neck area, chest, abdomen (majority), and pelvis
- managed by a multi-disciplinary team consisting of an oncologist, pediatric surgeon, pathologist, and radiologist
This tumor mainly occurs in children with an average age of presentation at 2.5 years. The infant type tends to be less aggressive; however, children aged over 12-18 months can have an aggressive form which may involve important structures in the body.
Signs and Symptoms
Symptoms vary based on the location of the tumor and may include:
- painless abdominal mass
- neck mass
- cough or difficult breathing
- Horner’s syndrome (drooping eyelid, unequal pupils, absence of sweating on one side of face)
- anemia and bruising
- bone pain
- fever
- bluish painless bumps (in infants)
- difficult walking or loss of bladder or bowel control
Diagnosing
The diagnosis is suspected based on a child’s physical exam and history. Some tests and bloodwork will be done to confirm the diagnosis. These may include:
- laboratory values including blood counts, kidney and liver function tests
- urine tests
- ultrasound
- CT scan
- MRI if concern for spine involvement
- nuclear imaging (MIBG)
- bone marrow evaluation
- possible biopsy
Treatment
This will be determined by the staging of neuroblastoma which is obtained by reviewing all the tests mentioned above. This is done to see if the cancer has spread in the body or is invading important structures near the tumor. Treatment could include one or some of these options.
- surgery to remove the tumor and any involved surrounding lymph nodes
- chemotherapy
- radiation therapy
- bone marrow transplant
- immunotherapy
Factors such as age, extent of disease, overall health of your child, and parental input will be reviewed by a multi-disciplinary team to provide the best care for your child.
Long Term
The prognosis for neuroblastoma is determined based on many factors as mentioned above. A pediatric oncologist will follow your child closely.
What is it?
This is a rare type of pediatric cancer involving the kidney, sometimes both kidneys. The kidney is an organ which helps clean the blood and make urine. They are located on either side of the spine closer to the back.
This type of tumor is malignant, as it can spread to other locations including the liver, lungs, and nearby lymph nodes.
Facts about Wilms tumor:
- It is the most common type of kidney cancer in children
- This type of tumor usually affects children under the age of 5
- About 500 children are diagnosed with Wilms tumor yearly in the United States
- It can be associated with certain syndromes
- All patients will be managed by a multi-disciplinary team which includes an oncologist, pediatric surgeon, pathologist, and radiologist.
Signs and Symptoms
Most children appear healthy since there are few early signs of this tumor. Wilms tumor is often found on physical exam by the parent while bathing or primary care doctor during a well-child exam.
Other symptoms may include:
- abdominal pain
- vomiting
- weight loss
- blood in the urine
- high blood pressure
- fevers
Diagnosis
If your physician suspects Wilms tumor, blood work and some imaging tests will be ordered. These may include:
- urinalysis
- complete blood cell count
- blood chemistry and liver function tests
- coagulation studies to ensure there are no bleeding risks
- ultrasound
- CT scan (sometimes followed by MRI based on results)
Treatment
Based on the results, the multi-disciplinary team will recommend the next step. The first step in treatment is usually surgery to remove all the involved tumor. This is called a radical nephrectomy. This involves removing the kidney with the tumor, the ureter (tube connecting to the bladder) and tissue surrounding the kidney with lymph nodes. Rarely, the tumor is so large or involving both kidneys and chemotherapy will be given before surgery.
The multi-disciplinary team will review the cells of the tumor and make recommendations regarding chemotherapy and possibly need for radiation once your child recovers from surgery.
Long Term
There will be regular visits with the oncologist for tests (blood work, ultrasound, or CT scan) to make sure your child remains healthy and the tumor is not returning.
WHAT IS IT?
Thoracic tumors include tumors in the chest cavity near the lungs, in the mediastinum (the space between the sternum and the spine), near the spine (paraspinal) and in the chest wall. These can be benign or cancerous tumors. The chest cavity is a common location for many secondary metastatic tumors arising from organs outside of the chest.
These tumors may include:
- Thymoma (mass of the thymus)
- Thymic cyst
- Thyroid tumors
- Lymphoma
- Teratoma
- Lung tumors
- Sarcomas of the chest wall
- Neuroblastoma
- Lymphangioma
- Bronchogenic cyst
SIGNS AND SYMPTOMS
A child with a thoracic tumor may have no symptoms. The signs and symptoms of a thoracic tumor may include:
- Shortness of breath
- Chest pain
- Fevers
- Inability to breath comfortably while lying down
- A chest wall mass
DIAGNOSIS
The diagnosis of a thoracic tumor is made with imaging which may include x-rays, CT scan or MRI. Laboratory tests may be ordered to help clarify what exactly is the tumor. Often a piece of the tumor will need to be obtained in order to allow a diagnosis to be made. This may be done with a surgery, either by taking out the entire tumor or just a small sample of the tumor, or by means of a needle using image guidance under the care of an Interventional Radiologist. Your doctors will work together to determine the best avenue to make a diagnosis.
TREATMENT
The definitive treatment of the tumor will be dependent on the specific diagnosis. It may involve observation, surgical excision, radiation therapy or chemotherapy. If surgical intervention is warranted, we will use minimally invasive techniques when appropriate and feasible.
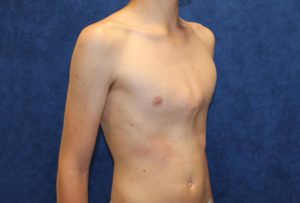
Chest Wall Deformities
Pectus excavatum and pectus carinatum are the most common chest wall abnormalities and are felt to be the result of abnormal growth of the cartilage that connects the ribs to the sternum (breastbone). It is not entirely clear why this abnormal growth occurs but some studies suggest that the genes that regulate collagen growth and remodeling are affected.
This poorly regulated growth may cause the sternum to push in resulting in pectus excavatum or it may cause the sternum to protrude which is termed pectus carinatum. The classification of these two diseases may be further defined by the degree of abnormality, the symmetrical or asymmetric growth of the cartilages, and the shape of the deformity.
Pectus excavatum and carinatum are 3-5 times more common in boys than girls. While there are some families where pectus abnormalities are seen in many family members, the majority of patients affected are the only member of their family to have the condition. Pectus abnormalities may occur in association with a number of different genetic disorders such as Marfan’s disease, Noonan’s syndrome, and many others or they may arise as an isolated finding.
Children with pectus abnormalities have a higher rate of scoliosis than the general population and almost all people with pectus excavatum have some degree of flaring of the lower ribs as well.
Aside from pectus excavatum and pectus carinatum, there are other rarer chest wall abnormalities such as Poland’s syndrome (lack of development of muscle and bone on one side of the chest and/or arm), Pouter Pigeon breast (abnormal sternal angulation, growth, and development), Cleft Sternum (in which the two halves of the sternum don’t join properly), and Sternal Foramen (in which there are one or more holes in the sternum).
The severity and associated symptoms of these other less common diseases will dictate the timing and appropriateness of repair.
Signs and Symptoms
Pectus excavatum may be present from infancy but more often is noted as a child reaches the first decade of life. The chest shape may change dramatically during growth spurts resulting in a larger defect over time.
Symptoms that patients with pectus excavatum often describe include chest pain, fast heart rate or palpitations, shortness of breath with exertion, and fatigue. From a physiologic standpoint, depression of the sternum with a loss of the front-to back distance of the chest may cause displacement of the heart to the left and rotation, mitral valve prolapse, decreased respiratory volumes and impaired excursion of the chest wall during breathing.
Perception of body image and self-esteem have been shown to be significantly lower in patients with pectus defects versus those without chest wall abnormalities. This may result in withdrawal from social and physical activities for these young people.
Depressed sternum with flaring of ribs associated with pectus excavatum.

Diagnosing
The diagnosis of pectus excavatum is usually made on the basis of physical exam, however the work up includes a CAT scan of the chest, an Echocardiogram to look at heart function, an electrocardiogram, and pulmonary function tests at a minimum.
From these tests an assessment of the severity of the chest wall depression and potential physiologic impact can be determined. If the CT index (a ratio of the transverse to the anteroposterior chest diameter) is greater than 3.25, then the defect is considered severe.
Studies of patients before pectus excavatum repair have been variable in their ability to demonstrate impaired preoperative cardiopulmonary function but in severe cases there is certainly impingement on the heart which may be associated with electrical and valvular problems as well as impaired lung function.
Post operatively, some of the large studies have shown a mild improvement in these parameters. Regardless of these results, most patients report improved exercise tolerance and feeling better after they have recovered from surgery.
Treatment
The repair of patients with pectus excavatum is usually done when the patients are approximately 12-16 years old with orthopedic pediatric surgery. This enables surgery before the chest becomes very rigid and is associated with less pain and fewer complications.
If surgical treatment of a pectus excavatum is pursued, there are 2 well tested surgical approaches.
The most common approach is the minimally invasive Nuss repair surgery which consists of 2 small lateral chest wall incisions for placement of a camera and passage of a metal bar into the chest, under the sternum, and out the other side of the chest. The bar is fitted to the appropriate chest shape of the patient and sometimes 2 bars are needed.
The bar is rotated so that the cartilage connecting the ribs and sternum are stretched into a new position and the bar is then fixed in place with sutures and a smaller stabilizing strut. Patients are kept in the hospital for several days to a couple of weeks depending on the severity of their pain and their mobility.
The bars are removed 2-3 years later as an outpatient procedure.
The Ravitch repair surgery is an open repair of pectus excavatum and is also used for several other chest wall deformities. In this operation a large incision is made on the front of the chest and the cartilage connecting multiple ribs to the sternum are removed on both sides. The sternum is partially divided and a small strut placed under the sternum. Drains may be placed under the skin and the incision is closed.
Each of these two approaches has advantages and disadvantages according to the type of chest wall abnormality and the decision of how to proceed is made in concert with the pediatric surgeon.
There are other experimental approaches to repair of pectus excavatum including the Mini-mover magnetic implant and the vacuum bell suction cup. If reports of these techniques prove consistently favorable, then they may be available at more centers in upcoming years.
Follow up care
After surgical treatment of pectus excavatum, patients will follow up in the office with their surgeon until the bar is removed 2-3 years later. Patients are not permitted to do contact sports for the first 3 months after surgery in order to let the chest heal properly and avoid shifting of the bar. Chest x-rays will be used to monitor the bar position during this follow up period.
If you have questions or concerns, please feel free to contact us for more information.
Signs and Symptoms
The heart and lung symptoms of pectus carinatum are usually less than those of excavatum but chest pain, reduced endurance, shortness of breath may be present. Due to the protruding nature of pectus carinatum, it is harder to conceal under clothing and therefore the social impact may be greater.
These chest wall abnormalities are most commonly asymmetric causing one side to push out more than the other giving the chest an unbalanced appearance. The cause of carinatum, like excavatum is felt to be related to abnormal growth of cartilage connecting the ribs to the sternum.
In pectus carinatum, the sternum and ribs protrude out due to imbalanced growth of cartilage.
Diagnosing
Pectus Carinatum is diagnosed by physical exam but a chest x-ray may be done if there is concern for other bony abnormalities. If the area of prominence is along the lower sternum (as noted in the picture above) it is called chondrogladiolar. If the prominent area is closer to the the upper chest near the sternum it is called chondromanubrial. Connective tissue disorders and scoliosis may also be present in patients with pectus carinatum as well.
Treatment
Recently, non-operative treatment with a brace has been utilized with good results in patients with pectus carinatum who have a non-rigid chest. This is why it is important that patients be seen for treatment of their pectus deformities before they have hit puberty and the chest loses its flexibility.
Treatment with a brace consists of being measured to determine where the pressure pads for the brace need to be and how best to fit the brace to the patient’s unique chest shape. The brace will need to be adjusted as the chest shape changes. Generally, the brace must be worn nearly continuously for at least 3-6 months in order to get the desired effect and once this is achieved, then the time of wearing the brace can be slowly decreased.
Complications from this approach are usually limited to skin injury or rash.
In cases where brace therapy is ineffective, the Ravitch approach to repair of the pectus carninatum yields good results. As described above, this consists of an operation where segments of the cartilage connecting the ribs to the sternum are removed and the sternum is divided. A plate is used to secure the new shape of the chest and it is removed as a second procedure months later.
Additional surgical techniques to correct pectus carinatum have been described in other countries including bar and plate fixation systems similar to the Nuss procedure and 2 bar sandwich compression procedures, however, these have not gained widespread acceptance in the United States.
A brace for pectus carinatum is custom-fitted to the shape of the patient and the areas that need compression.

Follow up care
After patients have undergone brace therapy they are seen back in the surgical office to monitor their progress and if it is unsuccessful to talk about surgical options with the family. After surgical repair, patients are seen over the next year to check on their progress. After surgical repair, patients may not engage in contact sports for 3 months in order to enable healing of the chest.
The surgeons of Austin Pediatric Surgery are happy to talk to you and your child about the various types of pectus chest wall abnormalities and discuss whether surgical or non-operative options are right for you.
At Austin Pediatric Surgery, we offer complete care for the pediatric patient with a pectus deformity through our Pectus Program. Dr. Erich Grethel, as the lead of our Pectus Program, has worked to optimize the perioperative care for our pectus patients, enabling the use of advance pain control techniques resulting in shorter hospital stays. Please call for an appointment at any of our clinic sites.
BIBLIOGRAPHY:
Nuss D, et al . Congenital Chest Wall Abnormalities. In Ashcraft’s Pediatric Surgery (5th edition).
Inflammatory Bowel Disease
What is Inflammatory Bowel Disease (IBD)?
Inflammatory Bowel Disease (IBD) is an immune-mediated inflammation of the intestine. The exact cause of IBD is not known. Recent theories favor an interaction of genetic predisposition, with altered intestinal bacteria, and environmental factors. More than 150 gene alterations have been noted to be associated with development of IBD. Antibiotic use, diet, and even Vitamin D exposure may be playing a role in the development of IBD.
The incidence of IBD in pediatric patients in the US and Canada is approximately 10 per 100,000 children and this rate appears to be increasing. IBD appears to be a much worse problem in developed countries than under developed countries suggesting the strong role of dietary and environmental factors. Care of pediatric patients with IBD requires a multidisciplinary team of doctors to ensure that they are treated effectively while maintaining the child’s ability to grow and flourish.
IBD is broken down into 3 subtypes, Crohn’s Disease (CD), Ulcerative Colitis (UC), and IBD Unspecified (IBDU).
The symptoms and management differ for these different subtypes and are outlined below.
What is Crohn’s Disease?
Crohn’s disease is an inflammatory process that may affect any part of the gastrointestinal tract from mouth to anus. While the last portion of the small bowel (or ileum) is most often affected, the disease can be seen in every part of the intestine with normal segments in between the inflamed areas. It may be seen only in the colon (Crohn’s colitis) or only in the small intestine (Crohn’s enteritis) or a combination of the two and even in the stomach and esophagus.
Inflammation around the anus with abscesses and fistula may be the first symptoms of Crohn’s disease. The inflammatory process in Crohn’s disease involved the entire thickness of the bowel wall which may explain why patients with Crohn’s disease may develop tight strictures or scars in their intestine that causes a blockage.
Signs and Symptoms
The initial symptoms of Crohn’s disease in children vary greatly but may include anemia (low blood count), fatigue, weight loss, fever, chronic abdominal pain, throwing up, persistent diarrhea, rectal bleeding, ulcers in the mouth or perianal infection. Many children have symptoms for a long time before it is recognized to be Crohn’s disease.
IBD can also present with inflammatory problems outside of the gastrointestinal tract as well with skin, liver, eye, or kidney problems (Table 1).
Table 1. Extra intestinal Symptoms of Inflammatory Bowel Disease
Ocular
Uveitis
Episcleritis
Iritis
Conjunctivitis
Glaucoma
Retinal disease
Skin
Erythema Nodosum
Pyoderma Gangrenosum
Sweet Syndrome
Oral stomatitis
Musculoskeletal
Arthritis
Osteopenia
Ankylosing Spondylitis
Sacroiliitis
Peripheral arthopathy
Growth Failure
Liver
Primary Sclerosing Cholangitis
Autoimmune Hepatitis
Bile duct cancer
Cirrhosis
Kidney
Kidney stones
Blood
Anemia
Venous thrombosis
Coagulation abnormalities
Platelet problems
Heart
Endocarditis
Cardiomyopathy
Myocarditis
Diagnosis
Patients suspected of having Crohn’s disease often have symptoms that could be confused with infection, so the initial work up of these patients may focus on establishing that there is no infection. This is done by laboratory examination of the stool for various bacteria and parasites as well as baseline blood work to determine the degree of inflammation.
Blood tests specific for IBD have been devised and are often utilized but their accuracy in confirming the diagnosis is mediocre. X-rays, CAT scans, and MRI scans may be helpful to determine the extent of the intestinal involvement and whether there has been narrowing or blockage from Crohn’s.
Ultimately, an endoscopy to look for the characteristic pattern of the disease and to get biopsies of the intestines is necessary for diagnosis. This endoscopy is best done by a pediatric gastroenterologist who is part of the team that takes care of IBD patients.
Treatment
The goal of treating patients with Crohn’s disease is to enable them to live a symptom-free life and have normal growth and development. Most patients with Crohn’s disease are successfully managed medically with a variety of medications such as steroids, Azathioprine, Methotrexate, 5-ASA, or Anti-TNF immunomodulating drugs such as Remicade.
Surgery is reserved for those patients who have not responded to medical treatment or have developed complications from their disease. Approximately 14% of children who have Crohn’s will need surgery over the first decade from diagnosis.
The most common reason for a patient to need surgery for Crohn’s is that a portion of their intestine has narrowed and is partially or completely blocking the passage of fluid through the intestine. This may cause the child to have a lot of pain or bloating or difficulty growing.
This narrowed area can either be removed and the bowel put back together or sometimes the narrow area can be opened by connecting it to an adjacent piece of the intestine without removing any intestine.
This procedure is called a stricturoplasty. Surgery may also be indicated when an inflamed part of the bowel forms a connection to another inflamed piece of bowel. This is called a fistula and acts as a short circuit for the absorption of nutrients.
Occasionally patients with severe perianal Crohn’s disease also need surgery to drain the infection. The goal of any surgeon who has experience taking care of patients with Crohn’s disease is to preserve as much intestinal length as possible while ensuring that the symptomatic piece of the intestine is removed.
Complications
Most patients who undergo surgery for Crohn’s disease do well depending on their nutritional status before surgery. Any time a piece of intestine is removed, and a new connection made, there are small risks of leaking from that connection or recurrent Crohn’s and scarring in that area.
Depending on the degree of immune system compromise from medicines, wound healing problems can also arise after surgery. Sometimes after abdominal surgery, scar tissue can develop that can cause another blockage of the intestine. All these problems are solvable with proper care and attention by your pediatric surgeon.
Follow up
Once the diagnosis of Crohn’s disease has been established, patients are followed closely into adulthood. This follow-up is usually coordinated by the pediatric gastroenterologists as repeat endoscopy is often necessary.
Biomarkers for IBD such as fecal calprotectin are becoming more useful in helping predict how a patient is responding to treatment and whether additional medicines should be added. Surgical follow-up will include examinations in the office and X-ray tests if needed.
What is Ulcerative Colitis?
In contrast to Crohn’s disease, Ulcerative colitis (UC) is an inflammatory process that is predominantly in the inner mucosal layer of the intestine as opposed to being throughout the wall of the bowel. It also has a more limited distribution in the intestine.
Typically UC is confined to a portion of, or the entire colon, with minimal changes seen in the end of the small intestine. Except for this “backwash ileitis”, UC is not seen in the small intestine which is an important differentiator from Crohn’s disease.
Signs and Symptoms
Children with UC usually have abdominal pain and diarrhea, which is often bloody. Weight loss is a frequent finding as well. Like Crohn’s disease, symptoms that are outside of the intestine may also be seen (Table 1) and may be the presenting feature. Given that there is a genetic component to IBD, it is not surprising that a family history is often positive for IBD.
Diagnosis
The diagnosis for UC, like Crohn’s disease, ultimately will require endoscopy to both examine and biopsy the intestine. Prior to this, blood tests to assess for the degree of inflammation and whether any other body systems are affected are completed. X-rays and CAT scan or MRI are used less often with UC but may be helpful in determining the extent of disease in the colon or demonstrating that the small intestine is not involved.
Clearly distinguishing Crohn’s disease from UC is important as the treatment from a surgical standpoint is different.
Treatment
Like Crohn’s disease, patients with UC are managed with a variety of medicines as noted above to help control symptoms. New immunomodulating drugs are continually being developed to help these children.
In those pediatric patients who are not responsive to medical treatment, surgery can be curative. In the ileoanal pull-through procedure, the colon is removed, and a portion of the small intestine is then connected to a short remaining cuff of colon near the anus.
A pouch of small intestine may be utilized to reproduce the reservoir function of the rectum. This surgery may need to be done in several stages depending on the medical condition of the patient. Frequently this surgery can be done with a laparoscope rather than a large abdominal incision which saves the child from a large scar and a lot of pain.
Complications
After the colectomy and ileoanal pouch pull-through procedure, the body will take some time to accommodate to this new configuration and frequent bowel movements are common but decrease over time. Infection, leakage, or scarring at the connection point are small risks of this surgery. Thirty to 73% of patients develop inflammation of the pouch after surgery (pouchitis). Antibiotics and probiotics are often effective in reducing or resolving this inflammation.
In a small percentage of patients, persistent pouchitis may signify that a patient actually has Crohn’s disease rather than UC which is why differentiating these 2 disease processes is so important. Difficulty controlling bowel movements is also a small risk after this surgery. Despite these risks and potential problems, most patients after surgical repair of their UC are pleased with the result and report a good quality of life.
Follow up
Patients with UC should be followed closely at regular intervals. They are followed by both pediatric gastroenterologists and pediatric surgery to determine if they are developing any of the problems noted above and to ensure that they are growing and developing normally. In most cases, if a patient has had surgery, their medications can be decreased or stopped completely.
It is important that these patients be transitioned to adult providers who can continue to monitor them for extra-intestinal signs of IBD as well as development of tumors later in life that may be associated with IBD.
In some patients the clinical and pathologic findings are not clearly Crohn’s disease or Ulcerative Colitis. Inflammatory Bowel Disease Unspecified (IBDU) is the term given to patients who have features suggestive but not conclusive for either Crohn’s or UC. It is twice as common in pediatric patients than adult patients and may occur in up to 10% of pediatric patients presenting with IBD.
These children are managed medically similar to other IBD patients but often require less medical treatment to achieve a response. Surgical interventions are less common in patients who have been correctly categorized with IBDU.
IBD can be a difficult disease for both a child and their family. The surgeons of Austin Pediatric Surgery are committed to working with you and your child to help you make the correct decisions about surgery for their IBD. We are dedicated to providing the best possible care to get your child back to growing and thriving and just being a kid.
Gastrointestinal Surgery
What is appendicitis?
Appendicitis is the most common cause of belly pain in children resulting in surgery. It occurs when the appendix becomes blocks, inflamed and fills with pus. This blockage can be caused by lymphoid tissue, stool (fecalith), foreign body, tumor or parasites.
Signs and Symptoms
Children typically present with nausea, vomiting, loss of appetite, fever and belly pain which becomes localized to the right side of their abdomen associated with tenderness on palpation.
Diagnosis
Appendicitis is usually suspected on the child’s symptoms and physical examination. Lab tests such as a white blood count, CRP or uranalysis can be helpful. Abdominal X-rays, ultrasound, CT-scan, and MRI are additional studies that can be used to make a diagnosis.
Surgical Treatment
Treatment for appendicitis usually is intravenous fluids, antibiotics and surgery to remove the appendix (appendectomy). Appendicitis surgery in children is most commonly done laparoscopically. Most recently, antibiotics alone has been suggested to treat early appendicitis. However, there is still controversy about this type of treatment.
Complications of appendicitis
If appendicitis is left untreated, the appendix will eventually burst or perforate, spilling pus into the abdominal cavity which in time, will form an abscess. In this situation, a drain can be placed through the skin into the abscess with the aid of an ultrasound or CT-scan. The appendix may be removed at a later date. This is called an interval appendectomy and is done to prevent recurrent appendicitis.
Follow-up Care
Any follow-up or activity restrictions after surgery will depend on the type of surgery performed.
What is a Meckel’s Diverticulum?
A Meckel’s diverticulum is an outpouching in the wall of the small intestine. It is the most common congenital malformation of the intestine, occurring in about 2% of the population. The lining of the pouch is made up of either acid-secreting tissue(stomach) or pancreatic tissue.
Signs and Symptoms
Most people born with this condition do not develop symptoms. However, in those children born with the acid-secreting tissue type may present with abdominal pain or ulcers which can bleed, become inflamed or burst.
Children can also present with belly pain, nausea and vomiting, and a bloated belly from obstruction or blockage caused by the diverticulum.
Diagnosis
The child’s symptoms and physical examination of presentation will determine which lab tests or imaging studies are done. These may include a Meckel’s scan, CT-scan or endoscopy. A Meckel’s scan is a specific study that is used to detect acid-secreting tissue.
Surgical Treatment
A Meckel’s diverticulum that is causing symptoms should be removed. This pediatric surgery can be performed either via an open or laparoscopic approach.
Follow-up Care
Any follow up care or activity restriction after the surgery will depend on the surgery performed. Please contact us if you have any questions, or call your pediatric surgeon for any immediate concerns.
What is an Intestinal Obstruction?
An intestinal obstruction is when food or stool is unable to move through the intestine, causing the material to become backed up. It can occur from scar tissue (adhesions), congenital conditions, tumors, narrowing (stricture) or twisting (volvulus) of the intestine.
Signs and Symptoms of a bowel obstruction can include:
Belly pain, nausea and vomiting, bloated belly and no passage of gas through the rectum (flatus).
Diagnosis
Bowel obstruction symptoms can be similar to symptoms of inflammatory bowel disease, so tests may include abdominal X-rays, CT-scan, or contrast studies can be used to confirm a bowel obstruction.
Treatment
The initial treatment will require bowel rest (NPO-nothing by mouth), intravenous fluids, and a nasogastric tube (NGT). If the obstruction does not resolve, pediatric surgery will be necessary. Intestinal surgery in infants varies on the location and severity of the obstruction, so our team of pediatric surgeons, doctors, and nurses will be sure to explain the process in detail as needed.
Follow-up Care
Any follow up care or activity restriction after the surgery will depend on the surgery performed.
What is GERD?
GERD is common in children and is usually treated with conservative measures such as thickening the feeds in an infant or medications. GERD is the process where the stomach acid or food comes back up into the esophagus. Most children will out-grow GERD.
When GERD becomes unresponsive to medications or causes problems like poor weight gain or growth, respiratory symptoms or is associated with damage to the lining of the esophagus, pediatric surgery can help.
Signs and Symptoms of GERD in children can include:
Spit-ups, fussiness, difficulty feeding, vomiting, weight loss, cough, wheezing, choking or chest pain.
Diagnosis
Tests which can assist in the diagnosis of GERD include an Upper GI, Barium Swallow, Gastric emptying study, endoscopy, esophageal monitory or pH probe.
Treatment
In severe cases of GERD, a fundoplication or wrap can be offered. A fundoplication is usually done laparoscopically and involves taking a portion of the stomach and wrapping it around the lower esophagus. This “wrap” strengthens the lower esophagus to decrease how much acid or food comes back up into the esophagus.
Not uncommonly, a gastrostomy tube or button will be placed at the same time to assist in feeding the child. This tube or button is placed directly through the skin into the stomach. A laparoscopic gastrostomy tube or button can also be placed alone for oral dysphasia or difficulty swallowing leading to the aspiration of liquids or food into the lungs.
Follow-up Care
Any follow up care or activity restriction after the surgery will depend on the surgery performed. Please contact us if you have any questions or concerns about your child’s surgery.
Complex Thoracic Surgery
Our pediatric surgeons have extensive training and experience in surgery of the thoracic cavity. Conditions which may benefit from surgical consultation and management include the following:
Our pediatric surgeons have extensive training and experience in surgery of the thoracic cavity. Conditions that may benefit from surgical consultation and management include the following:
Congenital Pulmonary Airway Malformation (CPAM): These are conditions that infants are occasionally born with that may be diagnosed via ultrasound before birth. They include abnormal areas of lung that may contain cysts or poorly functional lung tissue (formerly CCAM -congenital cystic adenomatoid malformation), or lung tissue that is separated from the other portion of the lung (sequestrations).
These abnormal lung areas may cause breathing trouble, may become infected or potentially become malignant.Your surgeon will discuss with you the risks, benefits, and alternatives of removing a portion of the lung that contains the anomaly, as well as the appropriate timing of the operation.
Congenital Lobar Emphysema (CLE): CLE is a developmental anomaly of usually one lobe of lung, leading to that portion of the lung becoming over-distended and trapping air. This can lead to breathing difficulties as the affected piece of lung pushes the other lung and heart out of the way.
Children who are symptomatic from this condition may require pediatric surgery to remove the affected abnormal lung tissue.
Thoracic cysts and tumors: There are many growths in the chest that may benefit from surgical biopsy or resection. These are often found when evaluating other illnesses or they may contribute to breathing or swallowing difficulties.
Examples include bronchogenic cysts, duplication cysts, neurogenic tumors, teratomas, lymphomas, as well as other masses.
Thymomas/Myasthenia Gravis: The thymus is located in front of the heart. It may be involved in disease, whether it be abnormal growth or as part of a disease such as myasthenia gravis, a condition involving weakness of the muscles. Removing the tumor or, in some cases, the thymus with pediatric surgery may help to eliminate symptoms.
Empyema: Occasionally, an infection in the lung extends to the space around the lung. In some instances, the infection can prevent the lung from expanding fully and the child from breathing well. In these cases, a drainage procedure may help clear the infection, and sometimes surgery is required to facilitate healing.
Pneumothorax: Older children and teenagers may have chest pain that is the result of a pneumothorax, or collapsed lung. This condition occurs spontaneously and results in chest pain with breathing or difficulty breathing. Treatment involves placement of a plastic tube in the chest to evacuate the air that is located outside of the lung.
Often there is a problem with the architecture of the lung – blebs or bullae are present which are thin pieces of lung that may continue to leak and will cause the problem to recur. In these instances, surgery is indicated to remove the abnormal, leaking portion of lung and encourage the remaining lung to fill the chest cavity.
In most of the above cases, rather than making a large incision on the chest wall to remove a mass or an abnormal piece of lung, the surgeon can place a camera and telescopic instruments through a few small (1/4 inch) incisions. This pediatric surgery is often call video-assisted thoracoscopic surgery (VATS). The small incisions are helpful to minimize discomfort and scarring after surgery. Many children may have a tube placed in the chest after surgery for a day or two to drain off extra fluid and air. The majority of children recover quickly from all the above procedures and are discharged home feeling well without any long-term effects or activity restrictions in 1-3 days.
Neonatal Surgery for Fetal Diagnoses
Our pediatric surgeons have extensive training and experience in surgery of the newborn infant. In addition, we consult with and evaluate mothers who are carrying a fetus with surgical conditions. We can help families plan for a variety of surgical problems that may be known before the child is born.
Conditions which may benefit from surgical consultation and management include the following:
Gastroschisis: A condition in which the abdominal wall does not form correctly, resulting in the intestine and internal organs protruding outside the abdomen. This condition occurs in about 1 in 2000-3000 births. It is most commonly not associated with other birth defects.
Often gastroschisis can be diagnosed before birth, and the surgeon can help you and your doctors tailor your birth plan. This is a condition that requires a surgical correction. This procedure may be performed in the infant’s nursery crib immediately after birth, or may require a more extended approach, wherein a plastic casing is used to cover the bowel for a period of days before the abdomen can be closed.
After the repair, the intestine in these infants sometimes takes a long time to “wake up,” and many may stay in the hospital for up to a month or more. Our pediatric surgeons are involved in studies investigating the best method of repair for these infants that will result in fewer infections, earlier feeding, and earlier discharge to home.
Omphalocele: Like in gastroschisis, the abdominal wall does not form correctly, though this condition is different in that the abdominal organs are most often covered with a membrane.
Surgical correction is ultimately necessary, though the timing is variable, and can occur within days of birth, to months or even a year or more depending on the size of the defect.
Newborns with omphalocele often have associated problems, such as genetic anomalies, lung development difficulties or kidney problems. Surgical correction of the omphalocele defect is just one aspect in the care of these medically complex infants.
Congenital Diaphragm Hernia: A problem in early development of the diaphragm can result in a congenital diaphragm hernia (CDH). The barrier between the chest and the abdomen is compromised, with intestine and other abdominal contents moving into the chest.
The spectrum of CDH is extensive, with some infants born with normal breathing and others who have severe restriction in lung development.
In conjunction with the neonatology team, the surgeons will help to resuscitate the infant. Some infants with severe lung disease benefit from extracorporeal membrane oxygenation (ECMO).
This involves the surgeon placing special large catheters in the blood vessels of the patient to initiate a form of heart-lung bypass. Repair of the diaphragm defect is necessary as well and is usually performed when the infant is strong-enough for surgery.
Children with CDH often will need surgical care and monitoring long after the immediate neonatal period. Our surgeons will follow these children and help address breathing difficulties, feeding problems (including reflux, oral aversion or bowel blockages), hearing or developmental struggles, and more.
Congenital Pulmonary Airway Malformations (CPAM): These are conditions that infants are occasionally born with that may be diagnosed via ultrasound before birth. They include abnormal areas of lung that may contain cysts or poorly functional lung tissue (formerly CCAM -congenital cystic adenomatoid malformation), or lung tissue that is separated from the other portion of the lung (sequestrations).
These abnormal lung areas may cause breathing troubles, or can contribute to infection problems or potentially become malignant.
If the lesions are causing distress to the infant in the newborn period, surgery can be performed to excise the lesion. Most infants with a prenatal diagnosis of CPAM or sequestration are initially asymptomatic. These infants are discharged home and can be evaluated for surgical intervention in the first few months of life.
Esophageal/intestinal obstruction: An ultrasound finding in a fetus can indicate that there is blockage of the intestinal tract, anywhere from the esophagus to the anus. These are generally not immediately life-threatening conditions at birth, but may require surgical correction in the first days of life after careful investigation of the newborn.
Our pediatric surgeons are specially trained to repair blockages or defects in the esophagus, stomach, small, and large intestine, as well as to repair anorectal anomalies. In some cases, the problem may be able to be repaired in a single setting. At other times, a staged repair is necessary, and the infant may need a temporary stoma – a piece of intestine brought out to the skin to allow the child to heal and grow.
Abdominal masses: A prenatal ultrasound may occasionally reveal a mass in the fetus’s abdomen. These are often difficult to specify before birth. The pediatric surgeon will discuss the findings with you and perhaps repeat the ultrasound or other imaging after the child is born. Often these findings disappear after birth, in other cases surgery will be necessary for diagnosis or treatment. Surgically treatable conditions range from cysts in the gall bladder/biliary tract, to the ovaries, to masses arising from the small or large intestine.
We will gladly consult for any prospective parents to discuss potential congenital anomalies identified by their obstetrician. Please contact us today to learn more.
Liver and Gallbladder Surgery
What is Pediatric Liver and Gallbladder Surgery?
The liver is an abdominal organ important for many reasons, including the formation of bile. Bile is needed for the digestion of fat. Bile is created in the liver, and stored in the gallbladder when it is not needed. Gallstones may form in the gallbladder, and these stones can cause abdominal pain. Bile ducts carry bile from the liver to the gallbladder and the intestines.
Pediatric liver or bile duct surgery may be necessary for many reasons. These include:
- Liver tumor
- For diagnosis of a liver disease
- Biliary atresia
- Choledochal cyst
Pediatric gallbladder surgery may be utilized to remove the gallbladder entirely if thought to be the cause of symptoms. Diagnoses which may require gallbladder surgery, or cholecystectomy, include:
- Cholelithiasis (gallstones)
- Cholecystitis (inflammation of the gallbladder)
- Biliary dyskinesis (a poorly functioning gallbladder)
Signs and Symptoms
Liver and gallbladder problems may present with abdominal pain, nausea, vomiting, or fevers. There may be yellowing of the skin or eyes. Children may have an abdominal mass. If you suspect your child may have a liver or gallbladder problem, please call your pediatrician and schedule an appointment immediately.
Diagnosis
Lab tests for liver function and enzymes may help diagnosis a liver problem. Tests such as ultrasound, CT MRI, or HIDA can be used to make a diagnosis.
Surgical Treatment for Liver or Gallbladder Disease
Pediatric liver surgery may be required for the diagnosis or treatment of a liver problem. This may require a biopsy or liver resection done through minimally invasive techniques or an open operation. The gallbladder can be removed with minimal consequences often through minimally invasive surgery.
Follow-up Care
Any follow-up or activity restrictions after surgery will depend on the type of surgery performed. If you have any questions or concerns, feel free to contact us or follow up with your pediatric surgeon.
The doctors of Austin Pediatric Surgery are pediatric surgical specialists for infants, children and adolescents. We are committed to providing state of the art pediatric surgical care for the children of Central Texas. We provide the full spectrum of surgical care, including the surgical treatment of diseases of the liver, bile ducts and gallbladder. Our team strives to make the surgical experience of our patients and families as safe and pleasant as possible.
Anorectal Malformations
What is it?
Imperforate anus (an anorectal malformation) is a newborn defect where the anus is absent. The anus is the opening to the rectum to allow stool to pass out of the body. Imperforate anus occurs in about 1 in 5000 births.
Types
- Anal opening is absent
- Anal opening is in the wrong position or too small to allow normal stool passage
- Absent anal opening and an abnormal connection (fistula) between rectum and urinary system or vagina
- In females, abnormal connection between intestine, urethra, and vagina called a cloaca.
Diagnosis
Newborns usually have a bowel movement in the first 48 hours of life. Doctors and nurses check for an anus immediately after birth and make the diagnosis on physical examination.
If the diagnosis is made, your doctor may order other test to rule out any associated anomalies
- Ultrasound to check for any kidney issues
- X-ray to check the intestine and spine
- Echo to evaluate the heart for any defects
Treatment
Surgery to correct the defect will be required. There are different options based on the type of imperforate anus.
Abnormal opening
This can be moved to the normal position with one surgery called an anoplasty.
Absent opening and low rectum
If no fistula is suspected, this can be done with one surgery called an anoplasty.
Absent opening and high rectum
This will require a three-staged surgical approach. First, a colostomy (part of the colon brought out through the abdominal wall) will be performed. The child will stool into an ostomy bag and go home to grow and get older for a few months before the next stage of surgery.
The second stage will be creating a new anus by bringing the rectum down to the normal position and possibly closing a fistula if present.
The third stage will be closing the colostomy to allow stool to pass normally from the rectum.
Hospital Stay
Your newborn will be able to go home when drinking well, having bowel function via the ostomy or neo-anus, and pain-free.
Post-operative
You will be taught how to take care of the ostomy or any diaper rash these babies are prone too. Most children with low rectum or abnormal opening have normal bowel function other than constipation; however, children with high rectum defects may have bowel movement difficulties requiring a bowel management program.
In addition to the usual post surgery instructions, your pediatric surgeon will advise you on the best way to keep your child during the healing process.
Pediatric Trauma
Pediatric trauma is a life-threatening injury to children, which requires hospitalization, and usually emergency surgery.
Austin Pediatric Surgery provides trauma care at Dell Children’s Medical Center of Central Texas. It is a Level 1 Pediatric Trauma Center, the highest designation available, meaning that our pediatric trauma surgeons are qualified and capable of handling even the more severe trauma cases.
Skin Masses and Infections
Skin Masses
A skin mass is any lump or bump which is just beneath the skin. These are most often benign, non-cancerous masses. The diagnosis of a skin mass is often made just through examining the child, but sometimes ultrasound can help make the diagnosis.
The list of possible diagnosis is long, but includes the following:
- Cysts
- Dermoid cyst
- Epidermoid cyst
- Pilonidal cyst
- Lymph node
- Pilomatrixoma
- Lymphatic malformation
- Vascular malformation
- Lipoma
- Neurofibroma
- Pyogenic granuloma
- Skin tag
- Rare liposarcoma
Depending on the suspected diagnosis along with the history and the exam of the patient, we may recommend excision or pediatric surgery. This is most often done under anesthesia, with the child able to be discharged to home on the same day of surgery.
The surgeons at Austin Pediatric Surgery would be happy to see your child to determine if surgery is recommended.
Skin Infections
Skin infections are common in children. Sometimes these infections can cause infected fluid to collect beneath the skin. These collections are called abscesses. If your child has an abscess, they will likely require surgical drainage of the abscess through a procedure called incision and drainage.
This is a brief procedure performed often under anesthesia. A surgical knife is used to cut a small hole in the skin and drain the infection. Often, a small rubber string is left in place as a drain. The wound can continue to be cleaned at home by soaking the area in warm soapy water.
Antibiotics may or may not be required to complete the treatment of the infection. If a drain is left in place, your child will need to return to our office 7-14 days after surgery for removal of the drain in the office. The surgeons at Austin Pediatric Surgery treat these types of infections daily and are well versed in their appropriate treatment.
Genitourinary
At Austin Pediatric Surgery, we have the expertise to treat genitourinary conditions such as undescended testicles, hernias and hydroceles. We also perform circumcisions throughout infancy to adolescence. Please contact us for additional information and to make an appointment.
Ovarian Mases & Cysts
As pediatric surgeons, we are trained to diagnose and surgically treat ovarian masses and cysts. Ovarian issues are generally diagnosed utilizing ultrasound, though they sometimes require MRI for detailed anatomic information. Austin Pediatric Surgeons are highly skilled in using minimally invasive laparoscopic surgery whenever possible to treat kids. Please contact us for additional information and to make an appointment.
